I-bronchitis enobungozi

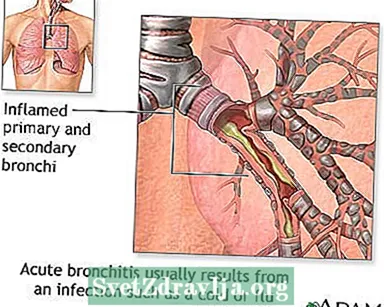
I-bronchitis ebukhali kukudumba kunye nezicwili ezitshayo kwiindlela eziphambili ezihambisa umoya ukuya emiphungeni. Oku kudumba kunciphisa indlela yomoya, nto leyo eyenza kubenzima ukuphefumla. Ezinye iimpawu ze-bronchitis kukukhohlela kunye nokukhohlela i-mucus. Acute kuthetha ukuba iimpawu zibekhona ixesha elifutshane kuphela.

Xa i-bronchitis ebukhali isenzeka, phantse ihlala isiza emva kokugula okubandayo okanye okufana nomkhuhlane. Usulelo lwe-bronchitis lubangelwa yintsholongwane. Ekuqaleni, ichaphazela impumlo, iisono, kunye nomqala. Emva koko isasazeka kwiindlela zomoya ezikhokelela kwimiphunga yakho.
Ngamanye amaxesha, iibhaktheriya zichaphazela ukuhamba kwakho komoya. Oku kuqhelekileyo kubantu abaneCOPD.
I-bronchitis engapheliyo yimeko yexesha elide. Ukufumanisa ukuba une-bronchitis engapheliyo, kuya kufuneka ube ukhohlela kunye ne-mucus kwiintsuku ezininzi ubuncinci iinyanga ezintathu.

Ezinye zeempawu ze-bronchitis ebukhali zezi:
- Ukungonwabi kwesifuba
- Ukukhwehlela okuvelisa i-mucus-i-mucus inokucaca okanye ityheli-luhlaza
- Ukudinwa
- Umkhuhlane - ngokuqhelekileyo uphantsi
- Ukuphefumla okufutshane kuya kusiba nzima ngomsebenzi
- Ukuqhaqhazela, kubantu abane-asthma
Nangona emva kokuba i-bronchitis ebukhali isuswe, unakho ukukhwehlela okomileyo, okuqhubekayo okuhlala kwiiveki ezi-1 ukuya kwezi-4.
Ngamanye amaxesha kunokuba nzima ukwazi ukuba unenyumoniya okanye i-bronchitis. Ukuba unenyumoniya, kunokwenzeka ukuba ubenomkhuhlane omkhulu kunye nokugodola, uzive ugula, okanye uphefumle kancinci.
Umboneleli wakho wezempilo uya kumamela izandi zokuphefumla emiphungeni yakho ene-stethoscope. Ukuphefumla kwakho kunokuvakala kungaqhelekanga okanye kurhabaxa.

Uvavanyo lunokubandakanya:
- I-x-ray yesifuba, ukuba umboneleli wakho ukrokrela inyumoniya
- I-oximetry ye-pulse, uvavanyo olungenabuhlungu olunceda ukumisela inani leoksijini egazini lakho ngokusebenzisa isixhobo esibekwe esiphelweni somnwe wakho
Uninzi lwabantu ALUFUNI ukubulala iintsholongwane kwi-bronchitis ebangelwa yintsholongwane. Usulelo luya kuhlala luhamba lodwa kwiveki e-1. Ukwenza ezi zinto kunokukunceda uzive ungcono:
- Sela amanzi amaninzi.
- Ukuba une-asthma okanye enye imeko engapheliyo yemiphunga, sebenzisa i-inhaler yakho.
- Phumla ngokwaneleyo.
- Thatha i-aspirin okanye i-acetaminophen ukuba unefiva. UNGABANIKI i-aspirin abantwana.
- Ukuphefumla umoya omanzi ngokusebenzisa i-humidifier okanye upheke igumbi lokuhlambela.
Amayeza athile onokuwathenga ngaphandle kokuyalelwa anokunceda ekuqhekezeni okanye ekukhululeni imicu. Khangela igama "guaifenesin" kwileyibhile. Buza usokhemesti uncedo lokuyifumana.
Ukuba iimpawu zakho aziphuculanga okanye ukuba uphefumla, umboneleli wakho unokumisela i-inhaler ukuba ivule iindlela zakho zomoya.
Ukuba umboneleli wakho ucinga ukuba unayo ibhaktheriya kwindlela yakho yomoya, banokumisela i-antibiotics. Eli yeza liza kususa kuphela ibacteria, hayi ii-virus.
Umboneleli wakho unokumisela amayeza e-corticosteroid ukunciphisa ukudumba kwimiphunga yakho.
Ukuba unomkhuhlane kwaye ubanjwe kwiiyure zokuqala ezingama-48 emva kokugula, umboneleli wakho unokumisela amayeza antiviral.
Ezinye iingcebiso zibandakanya:
- Musa ukutshaya.
- Kulumkele ukutshaya okutshaywayo kunye nongcoliseko lomoya.
- Hlamba izandla zakho (kunye nezandla zabantwana bakho) rhoqo ukunqanda ukusasaza iintsholongwane kunye nezinye iintsholongwane.
Ngaphandle kokukhwehlela, iimpawu zihlala zihamba kwiintsuku ezisi-7 ukuya kwezi-10 ukuba awunasifo semiphunga.
Fowunela umnikezeli wakho ukuba:
- Yiba nokukhohlela kwiintsuku ezininzi, okanye ube nokukhohlela okuhlala kubuya
- Bakhohlela igazi
- Unomkhuhlane ophezulu okanye ukugubha
- Unomkhuhlane ophantsi weentsuku ezintathu okanye ngaphezulu
- Unencindi eshinyeneyo netyheli-luhlaza, ngakumbi ukuba inevumba elibi
- Zive uphefumla kancinci okanye ube nentlungu esifubeni
- Unesifo esinganyangekiyo, njengesifo sentliziyo okanye semiphunga
- I-COPD-yintoni oza kuyibuza ugqirha wakho
- Sebenzisa ioksijini ekhaya-yintoni oza kuyibuza ugqirha wakho
 Amaphaphu
Amaphaphu IBronchitis
IBronchitis Oonobangela bronchitis etsolo
Oonobangela bronchitis etsolo Iimbangela ze-bronchitis engapheliyo
Iimbangela ze-bronchitis engapheliyo I-COPD (ingxaki engapheliyo yokuphazamiseka kwemiphunga)
I-COPD (ingxaki engapheliyo yokuphazamiseka kwemiphunga)
Amaziko oLawulo lweNtsholongwane kunye noThintelo lwewebhusayithi. Ukubanda kwesifuba (i-bronchitis ebukhali). www.cdc.gov/antibiotic-use/community/for-patients/common-illnesses/bronchitis.html. Ukuhlaziywa kwe-30 ka-Agasti ka-2019. Ifikeleleke ngoJanuwari 20, 2020.
UCherry JD. I-bronchitis enobungozi. Ku: UCherry JD, uHarrison GJ, uKaplan SL, uSteinbach WJ, uHotez PJ, ii-eds. Incwadi kaFeigin kunye neCherry yezifo ezosulelayo zabantwana. Ngomhla we-8. IPhiladelphia, PA: Elsevier; I-2019: isahluko 19.
UWalsh EE. I-bronchitis enobungozi. Ku: Bennett JE, Dolin R, Blaser MJ, ii-eds. Mandell, Douglas kunye neBennett's Principles and Practice of Infectious Diseases. Umhla we-9. IPhiladelphia, PA: Elsevier; 2020: isahluko 65.
UWenzel RP. I-bronchitis kunye ne-tracheitis. Ku: IGoldman L, iSchafer AI, ii-eds. Amayeza eGoldman-Cecil. Ngomhla wama-26. IPhiladelphia, PA: Elsevier; 2020: isahluko 90.

